Have you ever wondered why one child seems persistently impulsive and inattentive while another appears to swing from high energy and euphoria to deep irritability?
Behavioral challenges in children often lead to questions about diagnosis. In fact, global data suggests that around 5–7% of school-aged children are diagnosed with ADHD. On the other hand, the lifetime prevalence of childhood-onset bipolar disorder is much lower; studies place it around 0.1% to 2.5% in youth. In a clinical context, when a child is diagnosed with the stakes are high: treatment paths differ, risks of mood episodes of mania or depression differ, and long-term outcomes differ.
The challenge comes because symptoms of Pediatric Bipolar Disorder (PBD) and symptoms of (ADHD) overlap in ways that can mislead diagnosis. This article breaks down how to understand behavioral differences, common pitfalls, and key clinical features for parents, educators, and clinicians alike.
Defining the Disorders: Pediatric Bipolar Disorder vs ADHD
Pediatric Bipolar Disorder is a mood disorder characterized by distinct episodes of elevated or irritable mood (mania or hypomania) and depressive episodes in children and adolescents. The mood changes are more episodic, often dramatic, and represent a clear departure from the child’s baseline behavior.
In contrast, ADHD is a neurodevelopmental disorder marked by persistent patterns of inattention, hyperactivity, and impulsivity that are consistent across settings (school, home, social). In ADHD, the symptoms are more stable in timing and presentation rather than fluctuating in defined mood episodes.
Importantly, around 48% of youth diagnosed with Pediatric Bipolar Disorder are estimated to also meet criteria for ADHD. This overlap underscores why clear definitions and timelines matter.
Onset, Course, and Symptom Patterns
In Pediatric Bipolar Disorder, the onset often involves mood changes that swing from highs to lows, sometimes very rapidly, or mixed mood states (irritability plus hyperactivity). The course tends to be more variable, with periods of relative normalcy interspersed with mood episodes.
Some studies show children with bipolar disorder plus comorbid ADHD have earlier onset, more frequent episodes, and shorter periods of wellness. On the other hand, ADHD tends to present in early childhood (before age 12 by DSM criteria) and maintains a steadier pattern of inattentiveness, impulsivity, and hyperactivity across settings.
The key difference in behavior is the episodic extreme mood shifts in PBD versus the stable baseline of ADHD.
Key Behavioral Differences to Recognize
Here are some behavioral cues that help distinguish between the two conditions:
Mood elevation or extreme irritability: In Pediatric Bipolar Disorder, children may show elevated mood, grandiosity, decreased need for sleep, or markedly increased irritability. These features are less typical in ADHD.
Episodic nature: The child may go through distinct “episodes” of mood change in Pediatric Bipolar Disorder. ADHD symptoms are more consistent over time.
Inattention during mood episodes: While ADHD involves inattention as a primary feature, in Pediatric Bipolar Disorder, inattention may be secondary to mood state changes (mania or depression).
Sleep disruption: Major sleep patterns change, significantly less sleep without tiredness, or hypersomnia are more suggestive of Pediatric Bipolar Disorder.
Family history and severity: Youth with PBD may present with more severe symptoms, earlier onset, and a stronger family history of mood disorders.
Impulsivity and hyperactivity: These are central to ADHD, but when seen in Pediatric Bipolar Disorder, they may occur as part of a manic or hypomanic episode rather than as a baseline behavioral pattern.
Recovery intervals: In PBD, children may show more periods of wellness; ADHD tends to have persistent functional impairment unless treated.
Recognizing these behavioral differences is foundational in making the correct diagnosis and guiding effective intervention.
Overlap and Comorbidity: Why They Get Confused
The matter gets more complex because Pediatric Bipolar Disorder and ADHD often coexist and share some symptoms. Studies suggest that the comorbidity of ADHD in youth with bipolar disorder is high; one review estimated up to 48% in youth diagnosed with Pediatric Bipolar Disorder.
Meanwhile, children with ADHD have a higher risk of subsequently developing PBD than children without ADHD. The shared genetic vulnerabilities and overlapping neurobiology may explain the conjunction. What this means in practice is that clinicians must carefully map timelines, mood shifts, family history, and the nature of behavioral patterns rather than relying on one single symptom.
Misdiagnosis can lead to using treatments for ADHD when mood stabilizers would be more appropriate, or vice versa, which may worsen outcomes.
Assessment and Diagnostic Considerations
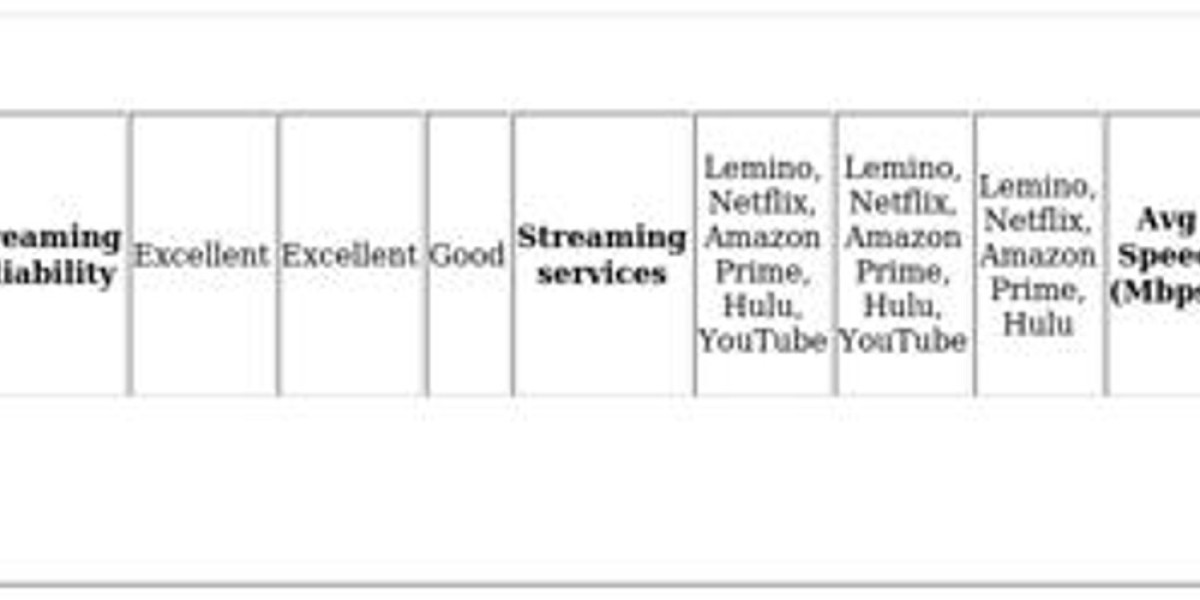
When evaluating a child for possible Pediatric Bipolar Disorder versus ADHD, the following diagnostic considerations are critical:
Timeline of symptoms: For PBD, look for clear-cut mood episodes, marked change from baseline, variable mood states. For ADHD, we expect consistent attention/hyperactivity issues across settings and time.
Context and severity: Mood episodes often disrupt functioning intensely in PBD and may require hospitalization. ADHD related impairment is more chronic but less episodic.
Sleep and energy changes: Drastic changes in energy, sleep and mood point toward Pediatric Bipolar Disorder. ADHD may have sleep issues but not the dramatic shifts.
Family history: A strong family history of bipolar disorder or mood disorders adds weight toward Pediatric Bipolar Disorder. Family history of ADHD supports the other side.
Response to treatment: ADHD often responds to stimulants and behavioral interventions. In contrast, using stimulants in undiagnosed Pediatric Bipolar Disorder may trigger mania or worsen mood instability.
Cross-setting impairment: ADHD requires symptoms in more than one setting (home, school). Pediatric Bipolar Disorder may have impairment tied to mood episodes, but may seem “normal” between episodes.
Rule out other causes: Other conditions, such as disruptive mood dysregulation disorder, anxiety, conduct disorder, and medical causes, must be considered, especially in mood irregularity.
Thus, a careful, longitudinal assessment is paramount, not just a snapshot of behavior.
Implications for Treatment and Support
Once the correct diagnosis between PBD and ADHD is established or if both co-exist treatment and support plans diverge significantly. For PBD, mood stabilizers, atypical antipsychotics and psychotherapy (family-based, cognitive behavioral) may be utilized to manage mood episodes and prevent relapse.
For ADHD, stimulant medication, behavioral therapy, classroom interventions, and organizational support are central. If misdiagnosis occurs, such as treating PBD as ADHD, outcomes can worsen, mood episodes may escalate, impulsivity may carrya higher risk, and functional impairment increases
Conversely, missing ADHD when present can leave inattention, school failure, and behavioral problems unchecked. Additionally, when both conditions are present (comorbidity), the treatment plan becomes more complex and often requires coordination among child psychiatrists, psychologists, educators, and the family.
Support strategies for both conditions also include educating families, working with schools to establish behavioral and academic accommodations, monitoring sleep and substance use (especially relevant in PBD), and tracking mood or attention patterns using diaries or apps. Early intervention, consistent follow-up, and tailored multi-modal support increase the likelihood of positive outcomes.
You may read Understanding Primary Membranous Nephropathy
Conclusion
Differentiating between ADHD is essential because each condition has distinct behavioral patterns, onset courses, and treatment needs. While children with ADHD typically exhibit persistent inattention, hyperactivity, or impulsivity, children with